Aortic Aneurysm Surgery
Westchester Heart and Vascular's Aortic Aneurysm team has the most combined experience in managing and treating complex aortic disease in New York and some of the most experience in the country.
Our team consists of international experts who write and speak around the world about their vast experience and expertise with all aspects of open and endovascular (stents) of the entire aorta, including valve-sparing root replacements, full aortic arch replacements, the use of hypothermic selective cerebral perfusion, thoracoabdominal replacements and many re-operative procedures.
What Is the Aorta?
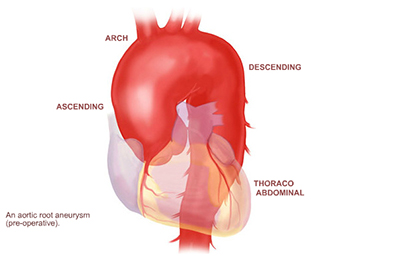
The aorta is the main blood vessel in the human body. As blood is pumped from the heart, it passes across the aortic valve, and then through the aorta, where it is then distributed through a system of smaller arteries. As the aorta travels through the body, each portion has a different name based on its location and each section supplies different organ systems or areas of the body. The aorta first leaves the heart and brings blood towards the head as the ascending aorta. As the aorta turns towards the left side of the body, it gives off branches to the upper body and the brain as the aortic arch. The aorta next travels down the chest, where it is called the descending aorta. The descending aorta continues through the abdomen as the abdominal aorta, where it supplies the abdominal organs before dividing to provide arteries for each leg (the iliac arteries).
The wall of the aorta is made up of three layers, the thin adventitia on the outside, the media, which is thicker and more elastic, and the delicate intima on the inside. The elastic nature of the vessel wall helps the aorta respond to the high pressures produced as blood is ejected from the heart.
Aortic Aneurysm Surgery Team at Westchester Medical Center
We have performed over 1,500 cases of Aortic Aneurysm Surgery, spanning the spectrum of aortic procedures, Bentall procedures, Ross procedures, including valve-sparing root replacements; full arch replacements, using hypothermic selective cerebral perfusion; thoracoabdominal replacements, using somatosensory and motor evoked potential monitoring; and many re-operative procedures. We are a referral center for acute aortic dissections for the Hudson Valley and have performed over 370 repairs for acute dissection. The overall mortality, for all aneurysm procedures, is 2.4 percent.
When appropriate, we employ a less invasive approach known as thoracic endovascular aortic surgery (TEVAR), which is used to treat an aneurysm or dissection in the upper aorta via a small incision. A stent graft is inserted to reinforce the aneurysm or dissection and prevent rupture.
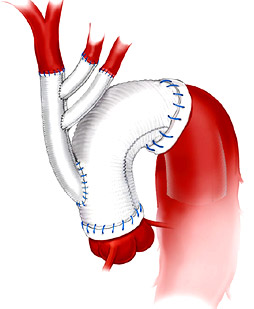
Dr. Spielvogel has lectured at national and international meetings on his method of aortic arch replacement, the trifurcated graft technique (below), which has been adopted internationally. For preoperative and postoperative aneurysm patients, we inaugurated an Aortic Aneurysm Follow-up Program that includes a cardiothoracic surgeon, cardiologist, a nurse practitioner and a custom-developed database to implement surveillance protocols for these patients. Currently, we follow over 1,500 patients with aortic disease. Junichi Shimamura, MD, our primary endovascular surgeon, and Igor Laskowski, MD, vascular and endovascular surgeon, are essential members of this team.
What Causes Aortic Aneurysms
Aortic aneurysms may result from a variety of predisposing conditions.
Degenerative dilation of the aortic wall is the most common cause of aneurysm formation. While the causes are not well understood, in some patients the elastic aortic tissue weakens prematurely, leading to progressive aneurysmal change.
Atherosclerotic disease may produce calcification in the wall of the aorta, and other blood vessels, which damages cells in the media, leading to subsequent dilatation. Poorly controlled hypertension, as it subjects the aortic walls to higher pressure, may also contribute to aneurysm growth. Atherosclerosis has been found to be related to such factors as elevated cholesterol levels, cigarette smoking, diabetes, poor physical conditioning, and genetic predispositions.
Genetic diseases, such as Marfan's Syndrome, Loeys-Dietz syndrome, Ehlers-Danlos Syndrome, and many other genetic non-syndromic disorders may lead to progressive dilatation of varying segments of the aorta due to abnormalities in fibrin, collagen, and other components vital to the integrity of the aortic wall.
Aortic dissections may result in chronic dilatation of the aorta over time. An aortic dissection is caused by a tear in the inner lining of the aorta which allows blood to track within the wall of the aorta. Acute dissections of the ascending aorta must be repaired immediately. Acute dissections of the descending aorta are often treated with minimally invasive endograft to prevent long-term aneurysm formation. Chronic dissections of the descending and thoracoabdominal aorta may be amenable to endovascular repair but often require open surgical repair if the aorta dilates over time.
Inflammatory conditions, such as Takayasu's arteritis, may lead to multiple arterial occlusions requiring reconstruction, while Giant cell aortitis may present with diffuse aneurysmal enlargement of the aorta.
Trauma, for example from motor vehicle accidents, may damage the wall of the aorta, leading to late aneurysm formation. Acute aortic transection related to severe trauma is treated with endovascular repair in the majority of patients. Care of the multi-trauma patient is coordinated with the Level 1 trauma team.
Bicuspid aortic valves patients represent one to two percent of the population. The presentation is variable. Some patients present in childhood with severe stenosis requiring surgical intervention. Other typical presentations include: young adult males with aortic root aneurysms with severe aortic valve insufficiency or older patients with severe stenosis secondary to degenerative calcifications. Forty to 50 percent of patients have an associated ascending aortic aneurysm at presentation.
Diagnosis
How Are Aortic Aneurysms Diagnosed?
An aneurysm is a localized dilatation of a blood vessel. Aneurysms may occur in any artery in the body, and in the aorta they may occur in any segment, whether in the chest (the ascending aorta, the aortic arch, or the descending aorta) or in the abdomen (the abdominal aorta). In a true aneurysm, the dilation involves all the layers of the walls of the aorta, in contrast to a pseudoaneurysm, or “false” aneurysm. In a pseudoaneurysm, the dilation does not involve all the layers of the aortic wall, but instead is usually contained by only the thin layer of adventitia.
There are many ways that doctors diagnose and follow aortic aneurysms. These different tests help to identify the presence of aneurysm as well as help determine treatment plans and follow up.
Chest X-ray
Often chest x-rays may suggest the presence of an aortic aneurysm. While they are not definitive studies, they may alert doctors of aortic pathology and suggest further tests.
CT Scan (Computed Tomography)
CT scan of the chest (often referred to as “CAT Scan”) is the preferred means of imaging aortic aneurysms, both at initial presentation and during follow-up. CT scans that focus on the aorta do require intravenous contrast (CT angiogram), which may be contraindicated in some patients with allergies or kidney problems. CT angiography is a critical tool for diagnosis, surveillance and surgical planning.
Echocardiography
Echocardiograms, whether transthoracic or transesophageal, may also help to provide further information about the aorta. Echocardiograms are of particular use when evaluating the ascending aorta, aortic valve, and the heart. Careful assessment of the aortic valve with transesophageal echocardiography determines the pathology and guides repair for valve sparing procedures.
MRI or MRA (Magnetic Resonance Angiography)
Magnetic resonance imaging (MRI) is another useful tool for examining the aorta. MRA exams have no radiation exposure and are well suited for screening and follow-up of aortic disease particularly in younger patients. The images obtained are similar to those provided by CT.
Does My Aortic Aneurysm Require Surgery?
The decision to replace the aorta is based on a number of criteria, namely symptoms, size, growth rate, and family history. This information applies to ascending aorta, aortic arch syndrome, descending thoracic aorta and thoraco-abdominal aorta.
Symptoms
The vast majority of aortic aneurysms are asymptomatic and are discovered as incidental findings during other imaging studies or related to a cardiovascular evaluation for other reasons.
In the setting of an ascending aortic aneurysm, chest pain is a concerning symptom and may prompt definitive urgent repair. If you have an aneurysm and are experiencing chest pain, you should contact your physician or the nearest emergency room immediately.
Size
While there is no absolute size cutoff, most surgeons will begin to recommend repair of ascending aortic aneurysms when they reach approximately 5 cm in size. For patients with Marfan’s Disease or other syndromic and non-syndromic inherited aortic aneurysms, surgery may be recommended for smaller sizes. Many factors are considered before recommending surgery; an evaluation by an experienced aortic surgeon is suggested. Patients undergoing cardiac surgery for other reasons, primarily those with bicuspid aortic valves, may require concomitant aortic replacement at smaller sizes. Patients with ascending aortic aneurysms greater than 4 cm should be followed with CT angiography or MRA at regular intervals to evaluate growth of the aneurysm, as directed by their physician.
Growth Rate
The rate of change in size of an ascending aortic aneurysm may also influence the timing of surgery. The faster the aneurysm grows, the sooner it should be repaired. Pain, often nonspecific, is considered a worrisome symptom and requires careful consideration in the decision to operate on small aneurysms.
Family History
Surgical repair may be recommended sooner based on a patient’s individual family history. Those with a history of genetic diseases, such as Marfan’s, Ehlers-Danlos, Loeys-Dietz, or other family history of aortic dissection (or sudden death with a known aortic aneurysm) may be candidates for surgical treatment earlier in their course.
Surgical Treatments for Aortic Aneurysm
Select a procedure below to learn more:
Graft Replacement
Used for Ascending Aorta
For ascending aneurysms that do not involve the aortic valve, simply removing the diseased portion of the aorta and replacing it with a tube graft is sufficient treatment. The aorta is usually replaced with a synthetic graft made of Dacron - a material which is strong and long-lasting. To perform the operation, the patient is placed on the heart-lung machine and the heart is stopped while the segment of aorta is replaced. The aneurysmal portion of the aorta is excised and the tube graft sewn to the remaining aorta.
Bentall Operation
Used for Ascending Aorta
For ascending aortic aneurysms associated with an abnormal aortic valve, the operation involves removing both the aorta and the aortic valve. Referred to as the Bentall Operation, both aortic valve and ascending aorta are replaced with a Dacron graft to which is attached a prosthetic aortic valve. As part of the operation, the coronary arteries are re-implanted into the aortic graft. This operation is also called an Aortic Root replacement.
Valve-Sparing Aortic Root Replacement (DAVID Procedure, Reimplantation Procedure)
Used for Ascending Aorta
In patients whose aneurysm involves the aortic root but whose aortic valve is either relatively normal or of sufficient quality to allow repair, this procedure may be used. The re-implantation procedure is a preferred option avoiding the risk of a prosthetic valve by preserving the native aortic valve. The ascending aortic aneurysm is resected and the coronary arteries mobilized. The aortic valve is supported by a Dacron graft and the coronary arteries are re-attached to the graft to complete the reconstruction.
Ross Procedure
Used for Active Young Patients with Aortic Valve Disease
The Ross procedure uses the patient's own Pulmonic valve and Pulmonic artery as an aortic valve substitute. The Pulmonary valve and Pulmonary artery are replaced with a preserved human donor valve. There are many benefits of the Ross procedure including: excellent hemodynamics for young athletes, avoidance of a prosthetic Aortic valve, avoidance of systemic anticoagulation and a favorable impact on long-term survival.
Freestyle Aortic Root Replacement
Used for Ascending Aorta
An alternative surgical approach, the use of a Freestyle porcine aortic valve and ascending aorta is utilized for patients with a small aortic root or infection. The surgical procedure is similar to the Bentall operation. The Freestyle prosthesis demonstrates excellent hemodynamics even in smaller sizes.
Trigraft Technique
Used for Complete Aortic Arch
For replacement of the aortic arch, we use a technique involving a Dacron graft with separate limbs for each of the arch vessels. This allows resection of the entire aortic arch and separation of each of the arch vessels supplying blood to the head and arms. Each of these vessels is then sewn to each limb of the trifurcated graft. The entire aortic arch is replaced with continuous brain circulation using hypothermic selective cerebral perfusion. This method minimizes the neurological risk with a very low stroke rate when compared to other techniques. The aortic arch is replaced with a separate graft, and, when complete, the trifurcated graft is connected to the arch graft. One of our faculty, Dr. David Spielvogel, was instrumental in the development of this technique, has extensive clinical experience with the procedure, and has published extensively on its use.
Open Repair
Used for Descending Thoracic Aorta, Thoraco Abdominal Aorta
The traditional method of repairing descending aortic aneurysms involves a left thoracotomy, which is an opening between the ribs on the left side of the chest. The aneurysmal aorta is excised, and a Dacron tube graft is sewn to the remaining aorta. For this operation, it is not usually necessary to stop the heart. When extensive resection of the thoracoabdominal aorta is necessary, deep hypothermia with selective brain and heart perfusion allows precise reconstruction of the aorta and important arterial branches. If stopping the heart is necessary we use deep hypothermia to protect end-organs and the spinal cord. Reducing the morbidity with extensive replacement of the thoraco-abdominal aorta is extremely important including protection of the spinal cord during repair. Extensive protocols to safeguard patients through the surgery and during their ICU stay enhance recovery and return to full function.
Endovascular Stent Graft Repair
Used for Descending Thoracic Aorta, Thoraco Abdominal Aorta
A newer type of aortic surgery has been introduced which repairs aneurysms from within the aorta using endovascular stent grafts. With this technique, there is no need for "open" surgery or cardiopulmonary bypass - the repair is performed entirely within the aorta itself (hence the term endo-vascular repair). By accessing the femoral artery in the groin, a graft is placed within the aortic aneurysm, effectively excluding that diseased segment of aorta. While not every patient is a candidate for this technique, it offers shorter recovery time, less pain, and faster return to normal activities.
Neurologic Protection
Prevention of stroke remains one of the central challenges in aortic surgery, and our practice takes numerous precautions to minimize the risk of neurologic complications. Strokes in complex aortic surgery may be the result of emboli (usually tiny particles of calcium or debris) which travel to the brain and cause damage.
Learn more about some of our strategies for neurologic protection.
Axillary Cannulation
As many patients with aortic disease have widespread atherosclerotic disease throughout the aorta, we routinely avoid using the ascending aorta itself for access for cardiopulmonary bypass. Our standard approach for aortic surgery uses the right axillary artery for connection to the cardiopulmonary bypass circuit, which has been associated with decreased embolic associated neurologic complications. An additional small incision under the right collar bone allows access to the axillary artery.
Selective Cerebral Perfusion
Modern techniques for reconstruction of the aortic arch allow continuous perfusion of the brain. At no time during the operation is the brain without blood flow. Hypothermic selective cerebral perfusion is the mainstay of the Trifurcated Graft technique, allowing safe repair with minimal neurological risk. The patient awakens promptly with early extubation and recovery.
Spinal Cord Monitoring and Protection
Modern techniques for reconstruction of the aortic arch allow continuous perfusion of the brain. At no time during the operation is the brain without blood flow. Hypothermic selective cerebral perfusion is the mainstay of the Trifurcated Graft technique, allowing safe repair with minimal neurological risk. The patient awakens promptly with early extubation and recovery.
CSF Drainage
We routinely place a catheter in the space around the spinal cord (an epidural catheter) which monitors the pressure of the cerebrospinal fluid (CSF) and allows us to drain fluid from the space if the pressure rises. This catheter is placed before the operation and left in place for approximately two days to maximize spinal cord blood flow and provide safe perioperative spinal cord monitoring and protection.
Distal Perfusion
During the operation, the patient is usually placed on a form of partial cardiopulmonary bypass support. This means of support allows the heart to continue to beat on its own, while maintaining blood flow and perfusion to the lower part of the body while the aortic replacement is taking place.
MEP / SSEP Monitoring
For all Descending and Thoracoabdominal aortic operations, we use professional neurologic monitoring that measures both motor and somatosensory evoked potentials (MEP / SSEP). A non-invasive monitoring system is in place throughout the surgery and allows the surgeon to be aware of any changes in the spinal cord function in real time. This facilitates changes in strategy during the surgery to lessen the risk of spinal cord damage.
Hypothermia
All descending aortic surgery is performed with the use of at least moderate systemic hypothermia, which involves cooling the patient, lowering metabolic work and decreasing the risk of neurologic injury.
Contact Us
For additional information please call 914.493.8793.
Our Addresses
Westchester Medical Center
Ambulatory Care Pavilion
100 Woods Road
Valhalla, NY 10595
117 Mary’s Avenue
Suite 105
Kingston NY 12401
Directions
By Car
By Train
Westchester Medical Center is served by Metro North's Harlem line via two stations:
- White Plains - Bus transfer options available
- Hawthorne - Taxi service available
For train fare and schedule information, call 1-800-METRO-INFO or go to www.mta.info
By Bus
There are three bus lines (Westchester Bee Line) you can take to our campus.
Please call 914.813.7777 for bus routes and fares.
Campus Map
The Westchester Medical Center campus includes the Maria Fareri Children's Hospital and the Behavioral Health Center.
Our Providers
- Cardiovascular Thoracic Surgery
- Cardiovascular Thoracic Surgery
- General Surgery
- Cardiovascular Thoracic Surgery
Ramin Malekan, MD
Associate Chief, Cardiothoracic Surgery
Associate Professor of Cardiothoracic Surgery
- Cardiovascular Thoracic Surgery
- General Surgery
Suguru Ohira, MD
Surgical Director, Heart Transplantation and Mechanical Circulatory Support and Director, Thoracic Aortic Research
Associate Professor of Cardiothoracic Surgery
- Cardiovascular Thoracic Surgery
- Cardiovascular Thoracic Surgery
- General Surgery